Hemolysis, Icterus and Lipemia: Understanding HIL Interference in Laboratory Testing
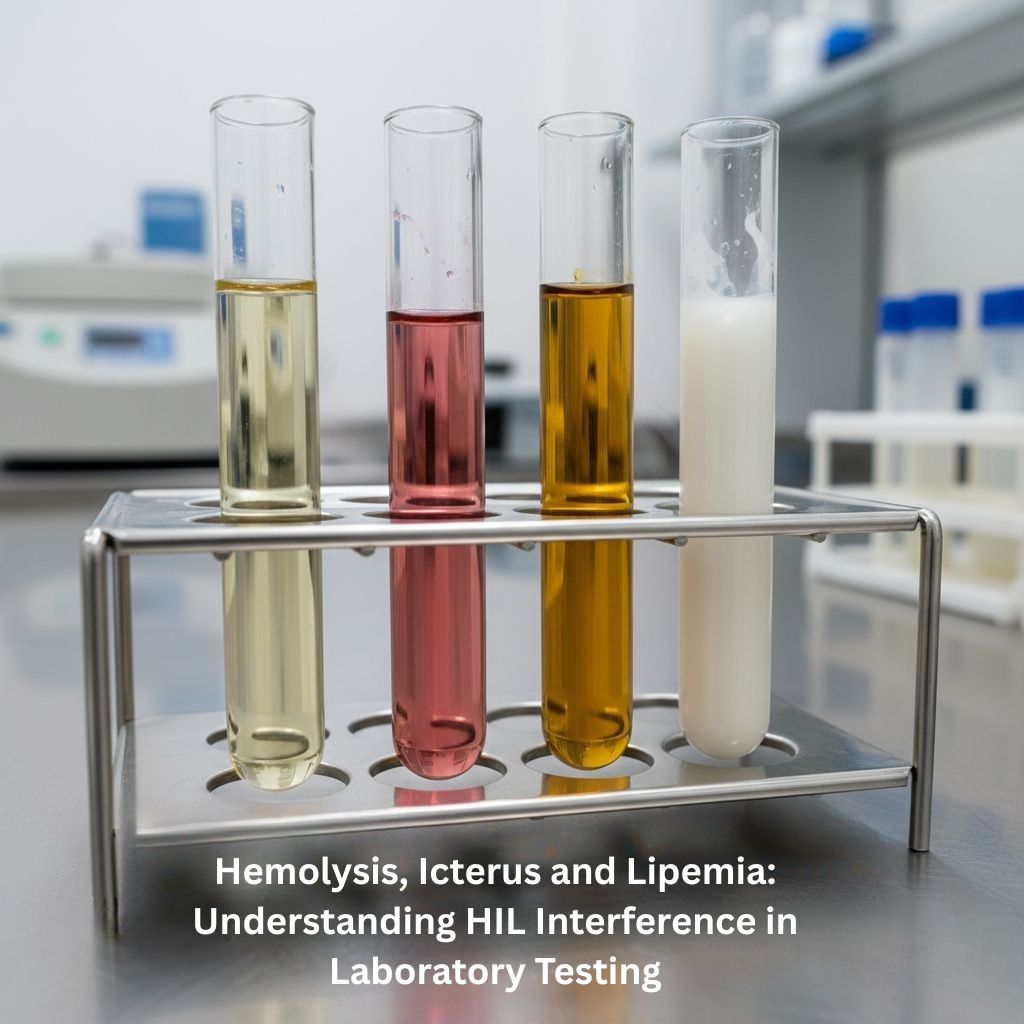
Accurate laboratory results are essential for effective diagnosis and treatment. However, several pre-analytical factors can compromise test accuracy. Among them, Hemolysis, Icterus and Lipemia collectively known as HIL Interference are the most common causes of inaccurate lab readings. These interferences alter the color, clarity, or composition of serum and plasma samples, leading to misleading biochemical results.
Table of Contents
ToggleHow Hemolysis, Icterus and Lipemia Interference Impacts Laboratory Testing
Even when advanced analyzers are used, the quality of the specimen remains the foundation of reliable results. HIL interferences affect how analyzers detect and interpret chemical signals.
🔴 Hemolysis
- Releases red cell components that alter test values and can falsely elevate electrolytes and enzymes.
🟡 Icterus
- Adds bilirubin pigments that absorb light in optical assays, affecting photometric measurements.
⚪ Lipemia
- Creates turbidity that scatters light and displaces plasma water, interfering with accurate readings.
Understanding each interference allows lab professionals to identify errors, repeat necessary tests, and ensure dependable results.

Understanding Hemolysis in Laboratory Samples
Hemolysis occurs when red blood cells rupture, releasing hemoglobin and intracellular substances into the serum or plasma. The sample may appear pink to red, depending on the degree of cell destruction. Hemolysis may happen inside the body (intravascular hemolysis) or outside the body (extravascular hemolysis) during blood collection or handling.
Causes of Hemolysis
Common causes include both in-vivo (within the body) and in-vitro (during collection) factors:
- Using too small a needle or excessive suction during collection
- Shaking or roughly mixing blood tubes
- Drawing from a site with IV fluid contamination
- Temperature extremes (freezing or overheating the sample)
- Delayed separation of plasma or serum from red cells
Hemolysis Index
The Hemolysis Index (HI) measures the amount of free hemoglobin in the serum or plasma and indicates how much red cell destruction occurred.
| Hemolysis Index Range | Interpretation |
|---|---|
| < 20 | No hemolysis |
| 20–100 | Slightly hemolyzed specimen |
| 100–300 | Moderate hemolysis specimen |
| > 300 | Marked hemolysis specimen |
Lab Tests Affected by Hemolysis
The release of intracellular components leads to false elevations or depressions in results:
- Potassium (K⁺) – Falsely increased
- Lactate dehydrogenase (LDH) – Elevated
- AST/ALT enzymes – Increased
- Bilirubin – Interference from free hemoglobin
- Troponin, CK-MB – Possible false positives
⚠️ Important Note
Because of these distortions, laboratories usually request a new sample if hemolysis is significant.
How to Prevent Hemolysis When Drawing Blood
Best Practices:
- Use the correct needle gauge
- Gently invert tubes, avoid shaking
- Avoid drawing from IV sites
- Store samples promptly at recommended temperatures
- Separate plasma or serum quickly
Hemolysis Workup in Clinical Settings
A hemolysis workup helps determine whether the issue is in vivo (true hemolysis in the patient) or in vitro (sampling error).
- Intravascular hemolysis: Free hemoglobin in plasma, low haptoglobin, elevated indirect bilirubin
- Extravascular hemolysis: RBCs destroyed in the spleen/liver, increased bilirubin, normal plasma color
Understanding Icterus in Laboratory Testing
Icterus refers to yellow discoloration of the serum, plasma, or body tissues due to excess bilirubin. The condition is often first noticed as scleral icterus, or yellowing of the whites of the eyes. In lab samples, an icteric blood sample can interfere with photometric tests because bilirubin absorbs light in similar wavelengths as many chemical reagents.
Causes of Icterus
- Liver dysfunction (hepatitis, cirrhosis)
- Hemolytic diseases increasing bilirubin production
- Bile duct obstruction blocking bilirubin excretion
- Drug-induced liver injury
- Neonatal jaundice due to immature liver function
Icteric Index
| Icteric Index Range | Interpretation |
|---|---|
| < 1.0 mg/dL | Non-icteric (normal) |
| 1.0 – 2.0 mg/dL | Mild icterus (slight interference) |
| > 3.0 mg/dL | Severe icterus (unreliable results) |
How Does Icterus Affect Lab Results?
Bilirubin interferes mainly through optical absorption:
- Can falsely lower glucose, cholesterol, and creatinine
- Affects enzyme-based assays such as AST and ALT
- Causes photometric interference in spectrophotometric analyzers
Managing Icterus Interference
Labs can reduce interference by:
- Using dual-wavelength (bichromatic) analysis
- Diluting samples to reduce bilirubin concentration
- Applying software corrections in automated systems
Icterus in Newborns (Neonatal Jaundice)
Neonatal jaundice is a frequent cause of icterus in newborns. The infant’s immature liver struggles to process bilirubin efficiently, leading to yellowing and possible lab result interference. Phototherapy helps break down bilirubin, and monitoring is crucial to ensure that test results reflect the baby’s true health status.
Understanding Lipemia in Laboratory Testing
Lipemia refers to excessive lipids or fats in the blood sample, causing the serum or plasma to appear milky or cloudy. It primarily occurs after a fatty meal or in individuals with hyperlipidemia. Lipemia affects spectrophotometric tests by scattering light and diluting the plasma water phase.
Causes of Lipemia
- Non-fasting samples (postprandial state)
- Hypertriglyceridemia (genetic or secondary)
- Parenteral nutrition (lipid infusions)
- Metabolic disorders (diabetes, pancreatitis)
Lipemia Index
| Lipemia Index Range | Interpretation |
|---|---|
| < 60 | Clear sample (non-lipemic) |
| 60 – 120 | Slightly turbid (mild lipemia) |
| > 120 | Cloudy or milky sample (marked lipemia) |
Effect of Lipemia on Test Results
Lipemic samples can cause several types of analytical interference:
- Light scattering leading to inaccurate absorbance readings
- Volume displacement causing falsely low electrolytes (Na⁺, K⁺, Cl⁻)
- Enzyme inhibition or poor reagent mixing
Reducing Lipemia Interference
- Ask patients to fast 10–12 hours before sample collection
- Ultracentrifugation to remove excess lipids
- Use of serum blanking in spectrophotometric tests
Frequently Asked Questions (FAQ)
Q1: What is hemolysis, icterus, and lipemia?
Hemolysis is when red blood cells break open and release their contents into the sample. Lipemia means the blood has many fat particles and looks milky. Icterus (jaundice) is excess bilirubin that makes blood and tissues yellow. These conditions can distort lab results, so labs report them.
Q2: What causes hemolysis interference for blood labs?
Hemolysis interference occurs when red blood cells rupture before or during testing and release contents that skew lab values. It’s usually caused by traumatic or improper draws, rough handling, temperature or transport problems, or in-body hemolysis from disease or drugs, and often produces falsely high potassium, LDH, AST, and bilirubin.
Q3: What causes lipemia in a blood test?
Lipemia occurs when blood contains lots of fat particles (mainly chylomicrons). Common causes are a recent fatty meal, very high triglycerides (genetic or from uncontrolled diabetes), IV lipid infusions, alcohol, or some drugs. Lipemic samples look milky and can distort test results; a fasting redraw usually fixes it.
Q4: What does it mean when a sample is icteric?
An icteric sample looks yellow-brown because it has high bilirubin. This usually comes from liver problems, blocked bile flow, or rapid red-cell breakdown. Icterus can interfere with some lab tests, so labs note it and doctors may investigate the cause.
Q5. Why does hemolysis cause icterus?
When red blood cells break down (hemolysis), they release hemoglobin that is converted into unconjugated bilirubin. If bilirubin production exceeds the liver’s ability to clear it, or the liver is damaged, bilirubin builds up. This buildup causes the yellowing of skin and eyes called icterus (jaundice).
Conclusion
In laboratory medicine, the integrity of every sample determines the accuracy of every diagnosis. Hemolysis, Icterus, and Lipemia remain the most significant pre-analytical challenges affecting clinical chemistry. Hemolysis alters enzyme and electrolyte levels by releasing red cell contents, while icterus changes optical readings due to excessive bilirubin pigments. Lipemia, on the other hand, introduces turbidity that scatters light and interferes with accurate measurement.
Understanding the hemolysis index, icteric index, and lipemia index allows laboratory professionals to recognize compromised samples and take corrective actions. By maintaining proper collection techniques, ensuring fasting conditions, and applying modern analyzer corrections, laboratories can minimize HIL interference and deliver precise, dependable results that truly reflect a patient’s physiological state. For more insights on clinical laboratory best practices and pre-analytical quality control, MFZ Clinical Lab provides comprehensive educational resources for laboratory professionals.
Recent Posts
- CBC Normal Range by Age and Gender: Unlocking CBC Test Results Made Easy
- Mitochondrial DNA Acts as a “First Hit” for Antibody-Mediated TRALI
- Iron Supplementation for Blood Donors Based on Ferritin Levels
- Hemolysis, Icterus and Lipemia: Understanding HIL Interference in Laboratory Testing
- Remote Lab Consulting: Shaping the Future of Virtual Healthcare
